Summary:
- Bangladesh inaugurates first skin bank at Dhaka’s National Burn Institute, using donor skin grafts to treat severe burn patients.
- Two children (2-year-old Hamida and 8-year-old Mariam) successfully treated with skin from four donors, showing reduced infections and faster healing.
- Living donors can contribute skin multiple times via localized anesthesia, while deceased donors’ skin must be collected within 6–10 hours postmortem.
- The facility aims to reduce mortality rates and expand access to advanced burn care, following models from Singapore and India.
Bangladesh inaugurated its first skin bank Sunday at Dhaka’s National Burn and Plastic Surgery Institute, marking a milestone in treating severe burn injuries. Special Assistant to the Prime Minister’s Principal Advisor, Professor Dr. Syedur Rahman, inaugurated the facility, which has already used donated skin grafts to successfully treat two critically burned patients.
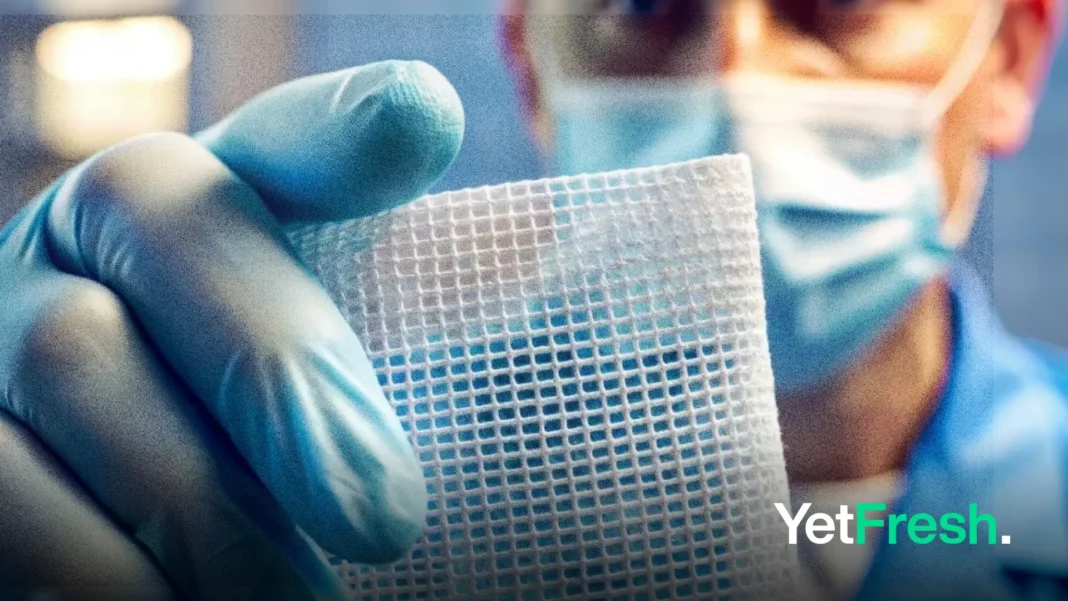
The skin bank, housed in Room 1239 of the institute, uses eight specialized freezers to preserve donated tissues. Four donors contributed skin for two recent transplants: a 2-year-old girl with 42% body burns and an 8-year-old girl with 22% burns. Both patients showed significant recovery after receiving grafts, including reduced infection risks and accelerated healing.
“Skin transplantation becomes critical when patients cannot provide enough of their own skin for grafts,” explained Dr. Shaon Bin Rahman, a resident surgeon at the institute. “Banked skin reduces mortality risks and stimulates natural tissue regeneration.” The facility follows protocols established in countries like Singapore and India, where skin banks have operated for years.
Living donors can contribute skin multiple times through a localized anesthesia procedure using a dermatome device, with full skin regeneration within 14 days. Deceased donors must have tissue collected within 6–10 hours of death, typically from the back or legs. “There are no legal barriers to donation, and the process is entirely safe,” emphasized institute director Dr. Maruful Islam.
Coordinator Dr. Mahbub Hassan highlighted the urgency of public participation: “Wider donor engagement could transform burn care nationwide.” Initial successes include treating Hamida, a toddler scalded by hot water, and Mariam, injured in a gas stove fire. Their mothers reported drastic improvements post-transplant.
The National Burn Institute’s initiative addresses a critical gap in a country where an estimated 300,000 annual burn cases often lead to preventable fatalities. With 123 staffed beds and rising demand, experts urge expanding the skin bank network to ensure accessible, life-saving treatments for all burn patients.